The Challenge
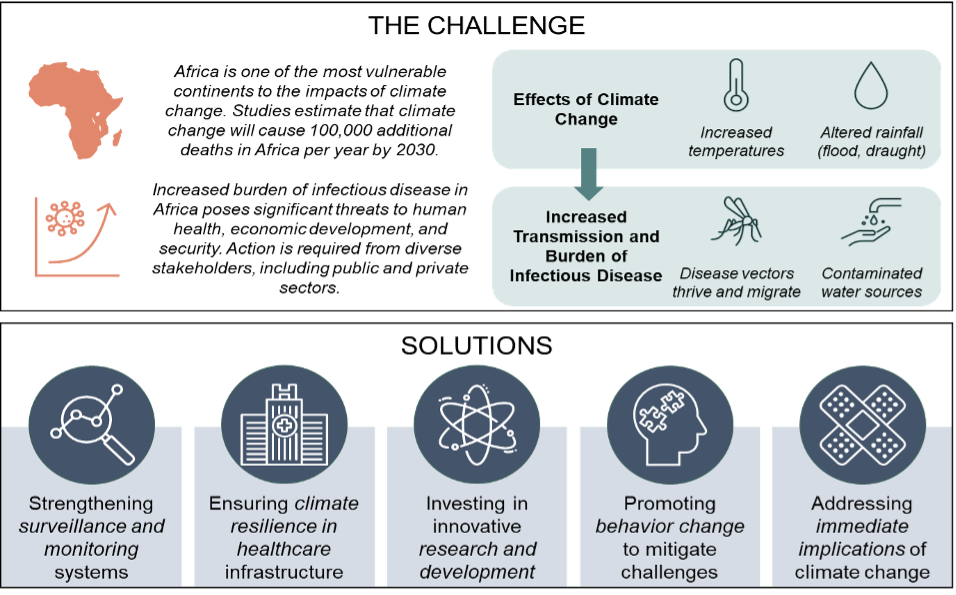
Africa is one of the most vulnerable continents to the impacts of climate change and is already experiencing symptoms of climate catastrophe such as increased temperatures, extreme weather events, rising sea-levels, and altered rainfall patterns. The impact of climate change on the health of Africans is significant, with some studies suggesting that climate change could cause an additional 100,000 deaths per year by 2030 [1]. Addressing the intersection of climate change and infectious disease in Africa requires urgent action by governments, the private sector, civil society, and international organizations. Further, climate change greatly exacerbates health problems on the continent, including the transmission of infectious diseases.
As climate change intensifies and the planet warms, infectious diseases—many of which are climate sensitive—are provided with the ideal environment to thrive as well as expand across geographies. Changes in temperature, rainfall patterns, and humidity are altering the distribution and behavior of disease vectors such as mosquitoes and ticks, thus increasing the prevalence and transmission of diseases such as malaria, dengue fever, and Lyme disease. As their natural habitats disappear, animal species are being forced to occupy new areas, which enables the potential spread of zoonotic diseases, both animal-to-animal, and animal-to-human—such as Ebola, Lassa fever, and Rift Valley fever.[2].
Flooding, also more frequent and severe due to climate change, can contaminate drinking water sources, further increasing the risk of waterborne diseases. We will then expect to see a rise in diseases such as cholera, typhoid fever, and hepatitis A through changes in precipitation patterns.
Solutions
It can certainly be discouraging and alarming to consider the possibility and preponderance of such dire outcomes, however, there are several policy, behavioral, resource, and systemic mitigations that can be put in place. Some have already risen to the level of urgent imperatives.
Strengthening surveillance & monitoring systems
Healthcare workers who are trained in disease surveillance, laboratory diagnosis, and outbreak response are crucial to the success of surveillance and monitoring systems. Information and communication technologies such as mobile phone technology, GIS mapping, and social media can also improve the efficacy of these systems.

Effective surveillance and monitoring systems are crucial in addressing the nexus of climate change and infectious disease in Africa. To enhance these systems, a comprehensive approach is required. Early warning systems that utilize real-time data, modeling, and risk assessments are invaluable in detecting the emergence and spread of infectious diseases. Furthermore, integrated disease surveillance and response (IDSR) systems that use standardized case definitions and reporting mechanisms enable the rapid detection of disease outbreaks through the tracking of cases by medical professionals and other stakeholders such as local health officials [3].
Public-private partnerships that bring together governments, the private sector, and international organizations to invest in disease surveillance and response systems are vital to effective disease control. So is improved data sharing across sectors such as agriculture, environment, and health will allow for earlier identification of potential outbreaks.
Furthermore, community participation in surveillance and monitoring systems is vital for strengthening surveillance and monitoring systems. Communities can be upskilled in recognizing and reporting disease outbreaks, and community health workers can collect data on disease trends. By bolstering surveillance and monitoring systems, we can promptly detect and respond to disease outbreaks, mitigating the impact of climate change on infectious disease transmission in Africa.
Ensuring climate resilience in healthcare infrastructure
Ensuring the climate resilience of healthcare infrastructure is imperative. As climate-caused extreme weather events become more frequent, infrastructure planning and strategies must meet the moment to mitigate the risk of infectious disease transmission. Some of the necessary actions include investing in water and sanitation systems able withstand climate change-induced impacts and weather events, construction of climate-resilient housing, and the promotion of renewable energy sources.

Healthcare facilities must be built and/or repaired and upgraded so that they may withstand climate-caused challenges, with updated building codes featuring climate-resilient design such as elevated floors, reinforced walls, and wind-resistant roofs. Backup power systems will ensure that healthcare facilities can continue to provide essential services during power outages. Addressing this deficit is of urgency given how many healthcare facilities in Africa are underdeveloped, lacking basic amenities such as clean water and sanitation [4]. Not only does this insufficiency makes delivering life-saving care an extreme challenge, it also further exposes patients and healthcare workers to infection and disease transmission.
To respond effectively to the health effects of climate change, healthcare workers must receive new training and updated equipment. This upskilling can range from education on how to diagnose and treat climate-sensitive diseases such as malaria and dengue fever to the management of extreme weather events such as heat waves and floods. Moreover, as we recall from the recent disparities around the COVID pandeminc, healthcare workers must imperatively be supplied with the proper personal protective equipment to safeguard themselves and their patients.
Investing in innovative research and development
It is essential to invest incrementally in the development and deployment of new technologies that can enhance healthcare delivery amid climate change. For example, remote diagnosis and treatment of climate-sensitive diseases can help to decrease the need for patients to travel long distances to receive healthcare. Digital health platforms also enable disease surveillance and response, allowing healthcare workers to promptly detect and respond to disease outbreaks [5]. Such investments can also help identify novel strategies for preventing and controlling infectious diseases.
Some innovations we need to see include research on the influence of climate change on disease transmission, the creation of new vaccines and drugs, and the evaluation of innovative prevention and control measures.Collaborations between the public and private sectors are also imperative in order to leverage resources and expertise in developing and implementing climate-resilient, innovative solutions that can address the health impacts of climate change.
Promoting behavior change to mitigate challenges

Education and awareness campaigns will encourage behavior change focusing on the risks of climate change and infectious disease. In the face of climate change and an increasingly interconnected world, it is imperative that individuals take proactive measures to reduce their risks. Such efforts can include handwashing, safe food preparation and storage practices, and other hygiene measures. Community engagement is critical in promoting behavior change, ranging from identifying local health needs to developing and implementing culturally appropriate health programs. Community health workers play an important role in delivering health education and promoting behavior change within their communities.
Traditional healers and community leaders also serve as resources for their communities, and their knowledge must be incorporated into future resilience design. Behavioral change can be incenvtiveed at the individual level, such as through rewards for households that adopt sustainable practices. Incentives can also be depoloyed at the community level, such as in encouraging widespread adoption of climate-resilient ag (drought-resistant crops, drought-sensitive irrigation, etc.). At the civic, regional, or national level, regulations and policies come into play in promoting systemic behavior change. Examples include clean energy requirements, or safe hygiene practices in healthcare facilities. Policies could also encourage sustainable farming practices, such as crop rotation and conservation agriculture.
Addressing immediate implications of climate change
Efforts to build climate resilience to reduce Africa’s vulnerability should also provide communities with basic amenities to weather the impacts of climate change. Amenities such as access to water and sanitation, electricity for productive use, clean cooking and climate-smart agricultural systems, and food preservation methods enable sustainable rural landscapes. Governments should encourage investment into standard primary health care centers to respond proactively to emerging infections through a “ONE Health [6]” approach.
Conclusion
The impact of climate change on the transmission of infectious diseases has been significant, leading to health, economic, and security implications. A comprehensive and multidisciplinary approach involving all stakeholders—governments, the private sector, civil society, and international organizations alike—is necessary to address this challenge. Actionable solutions including strengthening surveillance and monitoring systems, ensuring climate resilience in healthcare infrastructure, investing in innovative research and development, promoting behavior change to mitigate challenges, and addressing immediate implications of climate change. By taking urgent action, we can improve the health and well-being of people on the continent, reduce the burden of infectious diseases, and promote sustainable development.

The intersection of climate change and infectious disease is a global challenge, and solutions developed for Africa can be applied to other regions of the world facing similar challenges. There is an urgent need for increased investment in addressing this challenge in other parts of the world. This investment will improve the health and well-being of people in Africa, as well as contribute to achieving the Sustainable Development Goals, especially Goal number 3: Ensure healthy lives and promote well-being for all.
Additionally, the intersection of climate change and infectious disease represents one dimension of the interconnected impacts of climate change on all domains of life and society (e.g., agriculture, food systems, overall health, etc.). Solutions addressing this nexus should maintain perspective on the intersectional influences of climate change.
Dr. Chidiebere E.X. Ikejemba is the Director of Climate & Environment at Camber Collective. His body of work focuses on climate equity and justice, building resilient climate-smart development programs, strengthening political will for urgent climate change action and many other levers of activation. His theory of impact operates across both the upstream and downstream of a systems chain. that encompasses, just transition, agriculture & food security, migration, economic & rural development, climate education, waste management (circularity), healthcare, corruption and democracy, energy access, gender inclusion, carbon neutrality and other dimensions. The circularity of Camber’s approach and theory of influence is, we believe, the most congruous path to balancing economic reality and humanitarianism.
Notes
1 UNECA, “Climate Change and Health in Africa: Issues and Options,” United Nations Economic Commission for Africa, 2011.
2 E. S. Brondizio, J. Settele, S. Díaz and H. T. Ngo, “IPBES (2019): Global assessment report on biodiversity and ecosystem services of the Intergovernmental Science-Policy Platform on Biodiversity and Ecosystem Services,” https://doi.org/10.5281/zenodo.3831673, Bonn, 2019.
3 Kang G et al., “Improved surveillance of infectious diseases in resource-poor settings: The value of analytical epidemiology,” Emerging Infectious Diseases, vol. 20, no. 10, pp. 1728-1735, 2014.
4 Nguh BL et al., “Assessing the healthcare delivery system: A cross-sectional survey of healthcare managers and administrators in Cameroon,” Journal of Hospital Administration and Management, vol. 1, no. 1, pp. 1-11, 2017.
5 Mwapasa V et al., “The role of mobile health technologies in the fight against infectious diseases in low- and middle-income countries: a systematic review,” Journal of Medical Internet Research, vol. 20, no. 8, p. e10756, 2018.
6 ‘One Health’ is an integrated, unifying approach to balance and optimize the health of people, animals, and the environment. The approach mobilizes multiple sectors, disciplines, and communities at varying levels of society to work together. This way, new and better ideas are developed that address root causes and create long-term, sustainable solutions. One Health involves the public health, veterinary, public health, and environmental sectors. The One Health approach is particularly relevant for food and water safety, nutrition, the control of zoonoses (diseases that can spread between animals and humans, such as flu, rabies, and Rift Valley fever), pollution management, and combatting antimicrobial resistance (the emergence of microbes that are resistant to antibiotic therapy).
