
Digital technologies can bridge the gap between the current health care offering and the increased demand driven by population growth and urbanization. Combined with human-centered design techniques, digital tech can help center the patient experience decreasing the pressure on health care systems while improving both patients’ and providers’ experience. By prioritizing prevention over treatment, healthcare systems can also save more lives, leveraging digital tech’s ability to help patients to track their health, eat better, and check in more regularly with doctors through remote care when a trip to a facility is inconvenient or inaccessible. Furthermore, a human-centered design approach would enable policymakers to understand which services are the most needed and learn the realities and constraints of their patients.
The Covid-19 pandemic, recent rises in inflation, and the economic downturn have all increased pressure on healthcare systems. More than ever, every dollar matters. We believe that countries wishing to invest in tailored and intelligent health services, and who focus on increased productivity (and efficiency) will be more resilient to these and future challenges.
Centering the Patient Journey in Healthcare Design
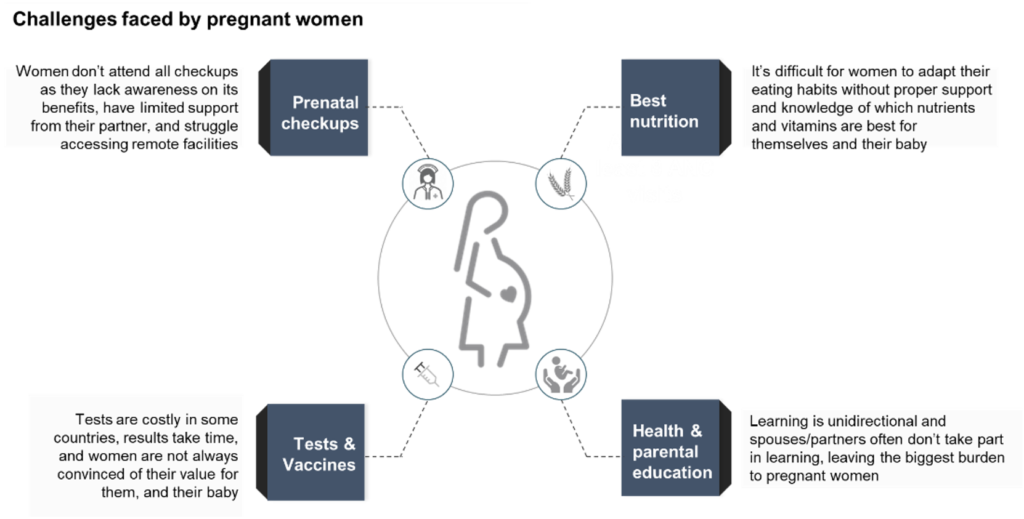
Countries will achieve higher positive health care outcomes if they put the context-specific needs, challenges, and beliefs of their patients at the center of future investments. Groups such as pregnant women, youth, or patients with chronic disease, for example, all have specific needs and encounter distinct friction points with the health care system.
In sub-Saharan Africa, pregnant women are particularly at risk. Indeed, 94% of all maternal deaths occur in the Global South.[2] Pregnancy necessitates many lifestyle changes and health care modifications; women must attend several ANC (ante-natal care) sessions to mitigate those pregnancy risks, and they must undergo regular health checks, comply with preventative medicine schedules, and adapt their nutrition habits. One study we analyzed across three sub-Saharan African countries revealed that only 44% of women attended regular antenatal checkups[3], with some women not seeing antenatal clinics early enough and others struggling to adhere to preventive treatment schedules. A deeper analysis showed that fear of being turned away, the constraints of social norms, and partner pressure are all factors which limit pregnant women’s engagement with ante-natal care services.
In order to design cost-effective solutions to increase the wellbeing of the mother and newborn, along with the efficiency of the entire health system, it’s necessary to deeply understanding what are the motivations and barriers specific patient groups experience. Below are examples of potential digital solutions that are simple to prototype and pilot and which demonstrate value-add and cost-effectiveness to global funders and private investors.

Mobile phones and internet access can be a game-changer in sub-Saharan Africa. The continent, on aggregate, enjoyed a mobile connectivity coverage rate of 81% in 2021.[4] With increased affordability of mobile phones, there already exists a sufficiently large base of patients to pilot these initiatives. Furthermore, as the share of adults accessing financial services in the Global South [5] it has become easier to build sustainable business models and monetize patient-centered health services. Once tested and scaled, such approaches could engender a virtuous cycle for the health systems of many countries in the Global South.
Enhance the Patient-Provider Relationship
While promising, digital tools aren’t meant to replace human interaction entirely; many patients want and need personal connectivity and a tactile experience in their heath care visit. Patient-centered solutions that engage and inform patients outside the facility can empower them to better understand and adopt providers’ counsel and also diminish the risks associated with unnecessary and/or harmful self-medication. At the same time, person-to-person contact enables providers to access individualized data, refine diagnoses, and increase empathy with patients. Face-to-face health care visits also provide a quicker feedback loop regarding the patient experience and the quality of care.
Prioritize Familiar Use-Cases for Vulnerable Groups
We believe policymakers should begin with several small experiments in order to test and better understand the needs of different patient groups. Combining qualitative human-centered approaches such as in-depth interviews, focus groups, and patient observation with quantitative methods including latent-class segmentation, discrete choice modeling, and patient data mining will provide comprehensive insights into patient preferences. Further, patient insights should be contextualized within the existing health infrastructure, so that care givers can obtain a comprehensive view of the opportunities and needs across the current infrastructure.
Organize for Scale
Countries face numerous challenges, from siloed initiatives that only partially scope the landscape and its opportunities, to the barriers of limited resources and buy-in. Therefore, delivering the expected results can be a challenge. Pulling all the innovation initiatives under the autonomous and lean oversight of a single organization is one way to increase efficiency and generate synergistic benefits. For example, a digital health ‘factory’ made of multi-sectoral expertise in health, public policy, design, and technology would enable countries to rapidly develop and test new prototypes and approaches. Once the business case is established, promising use-cases could scale to broader implementation with local and international partners.
Strengthen Local Partners
Trusting and empowering the local talent pool and working with local startups and service providers is a critical component of innovation acceleration. The “digital health factory” would be essential in building market-relevant business models that appeal to the private sector. At the same time, the public sector needs to de-risk its mechanisms in order to incentivize entrepreneurship into the sector. Ultimately, each country’s health system model will scale in its own specific context, taking into consideration the existing model, policies in place, and the maturity of the tech ecosystem. This said, the time for countries to experiment with innovation in the sector is now: doing so will leverage data and empathy alike to build resilient health systems that improve patient journeys throughout the continent.
[1] (PDF) Planning universal accessibility to public health care in sub-Saharan Africa (researchgate.net)
[2] Maternal mortality (who.int)
[3] Camber ANC analysis of recently pregnant women in Côte d’Ivoire, Cameroon and Malawi. 44% attending more than 4 ANC visits.
[4] The-State-of-Mobile-Internet-Connectivity-2021-Sub-Saharan-Africa.pdf (gsma.com)
[5] The Global Findex 2021: Interactive Executive Summary Visualization (worldbank.org)
