Despite the fact that the US spends approximately 18% of GDP on healthcare—almost twice as much as the average Organization for Economic Cooperation and Development (OECD) country—our healthcare system is riddled with problems, from widespread inequities to poor outcomes to barriers to care. In this three-part series, we discuss three specific types of barriers to care for those living with a serious mental illness—macroeconomic, legislative, and caregiver capacity—examining the nature of these access barriers and how they impact overall outcomes.
This first installment in the series is an exploration of a powerful macroeconomic barrier to mental healthcare in the US: an extreme workforce shortage driven by the fact that provider capacity is unable to meet the growing demand for services. We propose implementing an apprenticeship model as one way to help address the mental health workforce gap, though given the severity of the problem, it is important to note that a portfolio of solutions will be required.
The Mental Health Crisis
Mental health is an entrenched and growing public health crisis in the United States. Nearly one in four adults—approximately 58 million people—live with a mental illness.[i] Of those, over 14 million live with a serious mental illness (see Figure 1). Mental illnesses are disorders that affect a person’s thoughts, mood and/or behavior, and can range from mild to severe, whereas serious mental illnesses (SMI) substantially interfere with or limit a person’s daily life and ability to function[ii].
Many point to the 1963 Community Mental Health Act as the catalyst to the crisis, when people living with SMI were moved out of inpatient psychiatric facilities and into the community for care. Despite the well-meaning intentions of this act, community facilities were—and continue to be—vastly underfunded, leaving millions without the necessary support. Almost a third of all adults with a mental illness report that they are unable to receive the treatment they need.[iii] Key barriers to access include cost, insurance coverage and regulations, stigma, and workforce shortages. In this piece we will dive deeper into the workforce shortage challenge.
Figure 1. Prevalence of Mental Illness among US Adults
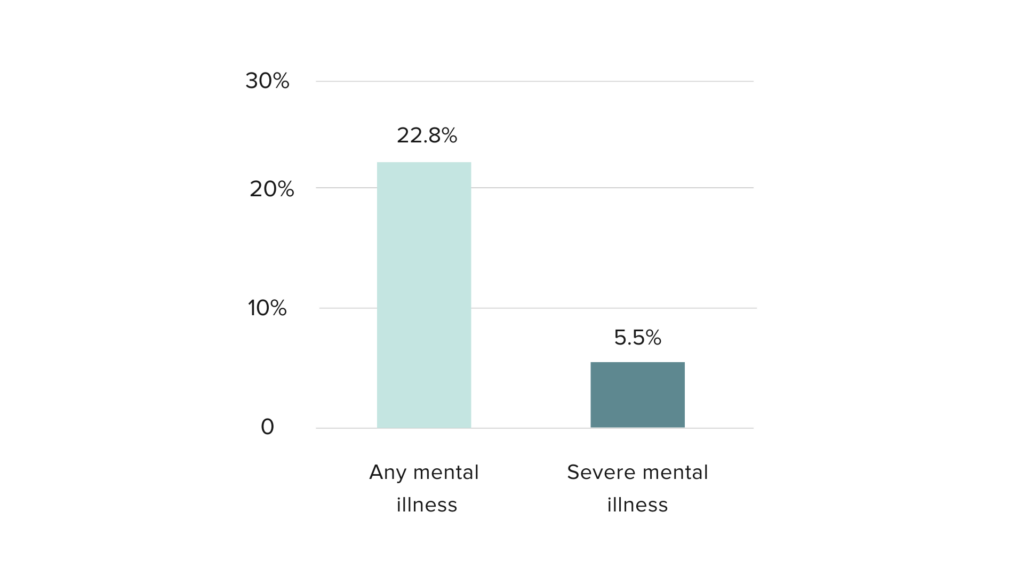
Source: National Institute of Mental Health (NIMH). “Mental Illness,” March 2023. https://www.nimh.nih.gov/health/statistics/mental-illness.
Demand is Outpacing Supply of New Entrants to the Workforce
The mental health workforce includes a wide range of providers, including the following:
- Licensed professionals, including psychiatrists, psychologists, and social workers
- Clinical support workers, such as aides and behavioral health counselors
- Community care workers, such as peer counselors and community health workers
- Frontline workers, such as law enforcement and emergency medical staff
Two forces are stretching provider supply: 1) growing demand for mental health services and 2) inadequate supply of new entrants into the workforce. Nearly half of all Americans live in mental health provider shortage areas.[iv]
As the US population has grown and the need for care has increased due to crises like the COVID-19 pandemic and substance use epidemic, mental health workforce growth has not kept pace. By 2026, the US will need approximately 900,000 mental health workers across all provider types to meet the demand for care, a 10% increase over current demand.[v]
While approximately half of states are projected to meet this demand, the other half are expected to experience a total shortfall of 55,000 workers—and this figure does not include the projected social worker shortages which we will turn to in the next paragraph. As the current workforce reaches retirement age or experiences burnout leading to a high churn rate, new entrants are not joining the workforce quickly enough to replace those exiting the field.
Shortages are particularly acute among licensed providers. Between 2009 and 2014, the number of psychiatrists relative to the population declined in 45 states, with this trend expected to continue through 2030.[vi] [vii] Similarly, shortages of social workers are emerging as they more frequently take on the behavioral care of clients, which increases caseloads without adequate workforce expansion.[viii] By 2030, 30 states will experience social worker shortages, totaling a shortfall of 200,000 nationwide.[ix]
Licensed providers such as psychiatrists and social workers must contend with expensive education, years of training, and high workloads. The growth of these professions is stymied by funding barriers and faculty retention challenges in training programs, which limit expansion and pose risks for existing programs.[x] Other positions that provide critical mental health support including psychiatric aides and community health workers, have fewer barriers to entry but often offer salaries so low that a family of four would qualify for Medicaid, which limits the pool of interested candidates.[ixi] [ixii]
For Americans living outside of major metropolitan regions, access to providers is even more limited. Rural counties have as little as one-third of the supply of psychiatrists and half the supply of psychologists compared to their urban counterparts (see Figure 2).[xiii] The lack of incentives to pursue a career in mental healthcare is exacerbated in rural areas. Barriers to rural provider recruitment include both lower salaries and limited benefits as well as place-based issues, such as incompatibility with the rural community culture and lack of infrastructure and amenities.[xiv] Inequities in availability of care intensify vulnerabilities already faced by people in these areas.
Figure 2. Psychiatrists and Psychologists per 100,000 People in Metropolitan vs. Non-Metropolitan Counties

Source: Variation in the Supply of Selected Behavioral Health Providers.” American Journal of Preventive Medicine, The Behavioral Health Workforce: Planning, Practice, and Preparation, 54, no. 6, Supplement 3 (June 1, 2018): S199–207. https://doi.org/10.1016/j.amepre.2018.01.004.
Along with an overall shortage of providers, there are inequities in racial and ethnic diversity among provider types, with higher paid roles like psychologists most often being held by white providers. The limited diversity of providers is concerning given that client-provider race and ethnicity concordance has been shown to lead to better treatment effectiveness in people experiencing SMI.[xv] While Black providers are strongly represented as social workers, counselors, and aides, the vast majority of psychologists and psychiatrists in the US are white (see Figure 3).[xvii], [xviii].
For People of Color, financial and educational barriers and workplace discrimination make entering or advancing in the field challenging. Furthermore, People of Color are more likely to remain in entry-level or lower paying jobs in healthcare and are underrepresented across healthcare profession schools both as students and faculty.[xviii] Expensive education, limited representation of People of Color in faculties, lack of culturally sensitive training and support programs, and biased licensure exams disadvantage students of color at every step along the education-to-career pipeline.[xix]
Expanding the mental health workforce, both in terms of sheer numbers and diversity, is critical to maximizing patient choice as well as the benefits from receiving care.
Figure 3. Mental Health Occupation by Race/Ethnicity
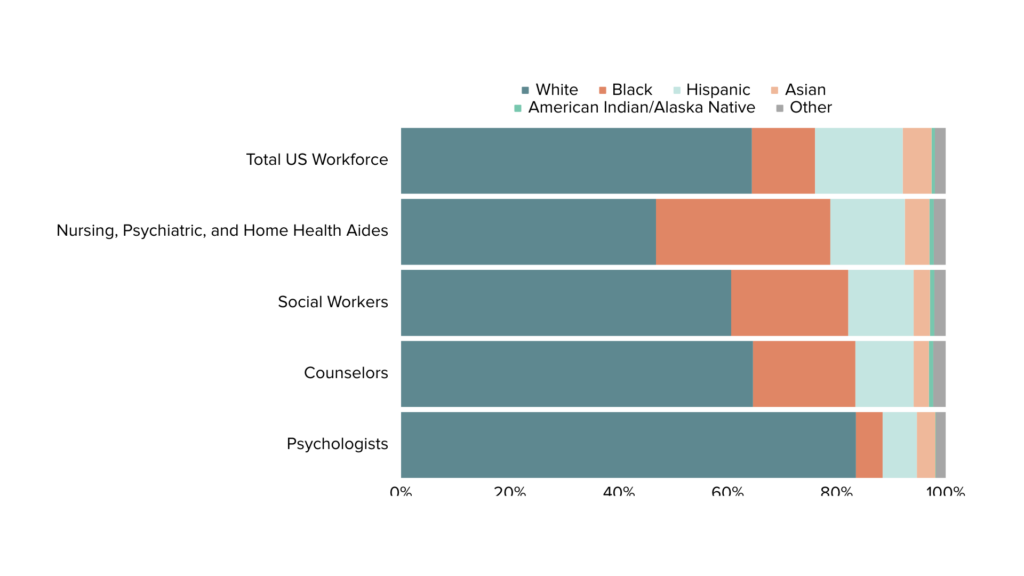
Source: US Department of Health and Human Services, Health Resources and Services Administration, National Center for Health Workforce Analysis. “Sex, Race, and Ethnic Diversity of US Health Occupations (2011-2015),” 2017. https://bhw.hrsa.gov/sites/default/files/bureau-health-workforce/data-research/diversity-us-health-occupations.pdf.
Impact of Mental Health Provider Shortages
The impacts of the mental health workforce shortages are profound, including the exacerbation of inequities, suboptimal patient outcomes, and higher costs for both individuals and the broader economy.
Already-long wait times for new appointments will continue to grow; a 2022 study found that the median wait time for a new patient mental health appointment was 67 days.[xx] Furthermore, out of pocket costs for patients often exceed their ability to pay, a situation intensified by the fact that too few providers accept insurance.[xxi] These limitations result in poorer outcomes for patients, as mild symptoms that go untreated may transform into severe presentations of mental illness. Downstream effects will likely emerge as untreated mental illnesses often lead to worse educational outcomes, lower earnings, and higher suicide rates. People of Color and people in rural areas will continue to be unduly impacted by premature mental-health related deaths because of inaccessibility of treatment.[xxii]
Serious mental illnesses were estimated to cost the US economy $318 billion in earnings losses, healthcare expenditures, and disability benefits in 2002.[1] [xxiii] While this figure is now more than twenty years old, the economic cost has likely only grown in recent years as a result of the increasing demand for and limited access to mental healthcare, in part driven by workforce shortages.
The US government spent $280 billion on direct mental health services in 2020.[xxiv] This number balloons when we consider the costs of treating comorbidities among people experiencing mental illness, which are estimated to be up to three times higher than for people without mental illness.[xxv]
Furthermore, myriad costs are not captured in this estimate of the economic impact of mental illness, as untreated mental health conditions also levy an undue burden on other systems, including social services, emergency departments, and law enforcement. The mental health workforce shortages will increase long-term costs as untreated mental illnesses grow more severe; sequelae (secondary conditions) develop, such as substance use disorders; and more people are unable to work because of their illness.
Addressing Mental Health Workforce Shortages
Increasing the number of new entrants to the field is critical to addressing the mental health labor force shortages, a stressor which is driving worsening mental health outcomes across the country. Expanding the mental health labor force will require both incentivizing professionals to enter the field and upskilling the workforce to increase capacity across provider types.
Proven Approaches: Training Capacity and Incentive Programs
Many states are moving quickly to update policies and deploy initiatives to address the workforce shortages, both across the system as a whole and specifically within mental health.
The Resident Physician Shortage Reduction Act of 2021 aimed to increase the number of residency positions for physicians, with a specific focus on increasing psychiatry positions. States like Pennsylvania and California have explored loan repayment and forgiveness programs for mental health providers to incentivize entrants and recruit to areas experiencing shortages.[xxvi], [xxvii]
Financial incentive programs have been shown to be effective at significantly increasing the number of healthcare providers working in underserved regions.[xxviii] These programs are especially useful for professions in which years of education and low- or unpaid clinical training are required, such as physicians and social workers. Standardizing incentive programs and expanding them nationwide is a critical next step to building the mental health workforce across multiple professional designations.
A More Novel Approach: Apprenticeship Programs
In addition to incentivizing new entrants through financial mechanisms and increasing residency training availability for physicians, a key solution to add to the quiver of options is an apprenticeship model for attracting, training, and employing additional mental healthcare workers.
Apprenticeship models for workforce development are used successfully across the globe.[xxix] Despite the fact that apprenticeships have existed in the US for some time, the system is often conflated with internships or assumed to apply only to trades rather than industries like healthcare.[xxx]
An apprenticeship model can increase mental health workforce recruitment and retention as well as candidate diversity. Through the removal of the financial barrier to education by compensating training, upskilling workers to enhance future compensation and workload capacity, and intentionally rolling out programming in rural and underserved areas, a mental health apprenticeship program could help address current and future workforce capacity constraints.
What is an Apprenticeship Program?
Apprenticeship programs can enhance mental health workforce recruitment and retention through the provision of high-touch, paid training. The basic structure of an apprenticeship program includes the vocational school, employer, and student. Students learn the theory and science of care work in the classroom and gain practical experience by directly applying what they have learned through a paid, supervised position (see Figure 4). A key benefit of apprenticeships is that they do not require prior tertiary education. Instead, education and workplace training are combined.
The apprenticeship model can be applied to a range of professional designations in the mental health workforce, especially upskilling clinical supports like behavioral health aides and community care workers like peer counsellors and community health workers. These roles can work in both the acute and emergent settings to address mental health crises and in long-term, ongoing care models such as group homes, homeless shelters, and residential visitation programs.
Some states are already implementing apprenticeship models, such as Washington’s program for behavioral health technicians and peer counselors.[xxxi] Others are offering apprenticeship programs adjacent to the mental health space, such as community health worker apprenticeships focused on populations that are unhoused.[xxxii] While the outcomes of these programs are not yet available, healthcare apprenticeship programs have shown promise in their ability to improve recruitment and retention of the provider workforce.[xxxiii]
Figure 4. Apprenticeship Components
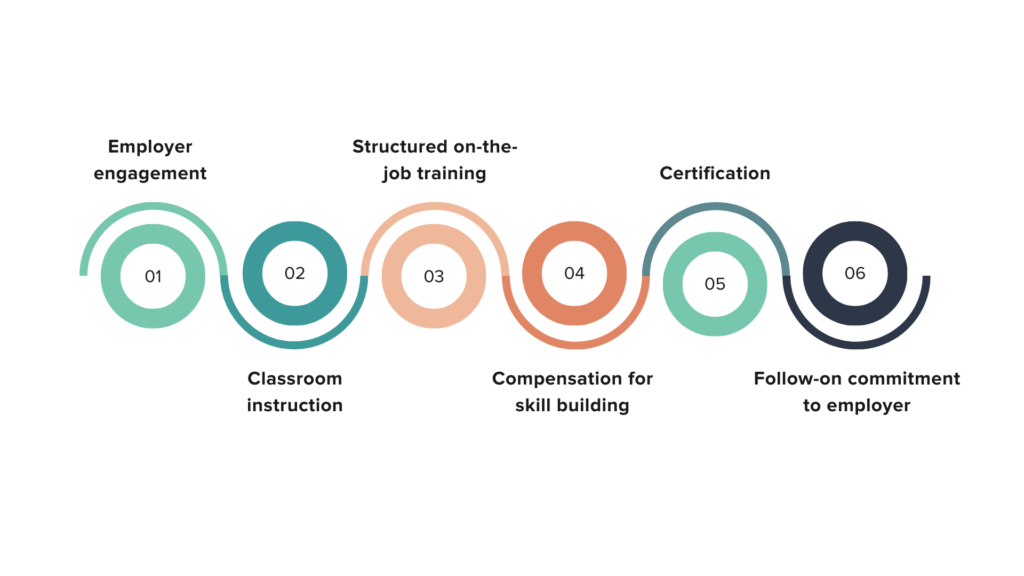
Source: The Workforce Connection. “Apprenticeships,” n.d. https://www.theworkforceconnection.org/apprenticeships/
An Apprenticeship Model Can Improve Mental Health Outcomes while Reducing the Burden on Providers
A robust apprenticeship program could address the mental health workforce shortages and increase access to care through three key mechanisms:
- Volume of providers: By incentivizing workers to enter training and integrating students immediately into the workforce, the number of providers available will increase.
- Diversity of providers: Apprenticeship programs can be designed to recruit candidates from diverse racial and ethnic backgrounds and across geographies to promote equitable representation of People of Color in the workforce and increase the number of providers practicing in rural and underserved areas.
- Task shifting: Training clinical support providers and community-based care workers to provide specific mental healthcare services can offload care work typically handled by psychiatrists, psychologists, and social workers where their expertise is not needed, thereby reducing wait times and costs.
Addressing the mental health workforce shortages will require a range of strategies to enhance capacity and improve provider diversity. Apprenticeships could rapidly and effectively increase the number of trained workers who can fill the gaps in care availability, thereby improving patient outcomes and reducing long-term costs. A strong mental healthcare workforce is key to ensuring people can manage mental illness and live their lives in a state of the best possible health and well-being.
Read Part Two
Kim Langenhahn draws on more than 15 years of consulting, operational, and startup experience in the domestic and international health and nonprofit sectors to help organizations navigate complex issues, operate more effectively, and deliver greater impact. During the course of her career, Kim has helped numerous healthcare organizations tackle a variety of strategic challenges such as scaling Terrapin Pharmacy’s remote medication adherence system, launching a MENA-focused healthcare incubator, devising system-wide strategy for the Saudi Arabian Ministry of Health as part of PwC’s consulting practice, and developing a market forecast for a pharmaceutical company alongside her L.E.K. Consulting colleagues. She is also the Cofounder of a small social enterprise that she runs with her family
Kim earned a Master of Business Administration and a Master of Public Policy from the University of Chicago as well as a Master of Science in Quantitative Management and a Bachelor of Arts from Duke University. An avid traveler, reader, bread baker, ice cream churner, and (aspiring) cheese maker, she also enjoys helping her husband tend to their rooftop garden and vermiculture operation. She currently resides in Washington, D.C.
Morgan de Luce is driven by a passion for health equity, human-centered design, and trust-based philanthropy. She has over seven years of experience working with nonprofits to improve access to healthcare and education for vulnerable populations. Prior to joining Camber, she led fundraising and operations for OASIS (Organizing to Advance Solutions in the Sahel) as well as managed the organization’s reproductive health medicines research portfolio. Prior to that, she worked in Kenya to improve children’s education access and career success with the organization Flying Kites.
Morgan received her Master of Public Health in Health and Social Behavior from the Harvard T.H. Chan School of Public Health, where she concentrated in Maternal and Child Health. Morgan also holds a Bachelor degree in Sociology from Boston College. In her free time, Morgan loves to practice yoga, experiment in the kitchen, and explore California’s many beautiful state parks.
Endnotes
[i] National Institute of Mental Health (NIMH). “Mental Illness,” March 2023. https://www.nimh.nih.gov/health/statistics/mental-illness.
[ii] Ibid.
[iii] Mental Health America. “The State of Mental Health in America,” 2023. https://mhanational.org/issues/state-mental-health-america.
[iv] Health Resources and Services Administration. “Health Workforce Shortage Areas,” October 2023. https://data.hrsa.gov/topics/health-workforce/shortage-areas.
[v] Bateman, Tanner, Sean Hobaugh, Eric Pridgen, and Arika Reddy. “US Healthcare Labor Market.” Mercer, 2021. https://www.mercer.com/content/dam/mercer/assets/content-images/north-america/united-states/us-healthcare-news/us-2021-healthcare-labor-market-whitepaper.pdf.
[vi] Mann, Sarah. “AAMC Research Confirms Looming Physician Shortage.” AAMC, September 2016. https://www.aamc.org/news/aamc-research-confirms-looming-physician-shortage.
[vii] National Center for Health Workforce Analysis. “Behavioral Health Workforce Projections, 2017-2030.” Health Resources and Services Administration, n.d. https://bhw.hrsa.gov/sites/default/files/bureau-health-workforce/data-research/bh-workforce-projections-fact-sheet.pdf.
[viii] National Center for Health Workforce Analysis. “Behavioral Health Workforce Projections, 2017-2030.” Health Resources and Services Administration, n.d. https://bhw.hrsa.gov/sites/default/files/bureau-health-workforce/data-research/bh-workforce-projections-fact-sheet.pdf.
[ix] Lin, Vernon W., Joyce Lin, and Xiaoming Zhang. “ US Social Worker Workforce Report Card: Forecasting Nationwide Shortages.” Social Work 61, no. 1 (January 2016): 7–15. https://doi.org/10.1093/sw/swv047.
[x] Pheister, Mara, Deborah Cowley, William Sanders, Tanya Keeble, Francis Lu, Lindsey Pershern, Kari Wolf, Art Walaszek, and Rashi Aggarwal. “Growing the Psychiatry Workforce Through Expansion or Creation of Residencies and Fellowships: The Results of a Survey by the AADPRT Workforce Task Force.” Academic Psychiatry 46, no. 4 (2022): 421–27. https://doi.org/10.1007/s40596-021-01509-9.
[xi] US Bureau of Labor Statistics. “Occupational Employment and Wage Statistics: May 2022 Occupation Profiles,” 2022. https://www.bls.gov/oes/current/oes_stru.htm.
[xii] HealthCare.gov. “Federal Poverty Level (FPL) – Glossary,” 2023. https://www.healthcare.gov/glossary/federal-poverty-level-fpl.
[xiii] Andrilla, C. Holly A., Davis G. Patterson, Lisa A. Garberson, Cynthia Coulthard, and Eric H. Larson. “Geographic Variation in the Supply of Selected Behavioral Health Providers.” American Journal of Preventive Medicine, The Behavioral Health Workforce: Planning, Practice, and Preparation, 54, no. 6, Supplement 3 (June 1, 2018): S199–207. https://doi.org/10.1016/j.amepre.2018.01.004.
[xiv] Schwartz, Malaika, Davis Patterson, and Rachelle McCarty. “State Incentive Programs That Encourage Allied Health Professionals to Provide Care for Rural and Underserved Populations.” Center for Health Workforce Studies, University of Washington, December 2019. https://depts.washington.edu/fammed/chws/wp-content/uploads/sites/5/2019/12/State-Incentive-Programs-Allied-Health-FR-2019.pdf.
[xv] Chao, Puihan J., John J. Steffen, and Elaine M. Heiby. “The Effects of Working Alliance and Client-Clinician Ethnic Match on Recovery Status.” Community Mental Health Journal 48, no. 1 (February 1, 2012): 91–97. https://doi.org/10.1007/s10597-011-9423-8.
[xvi] US Department of Health and Human Services, Health Resources and Services Administration, National Center for Health Workforce Analysis. “Sex, Race, and Ethnic Diversity of US. Health Occupations (2011-2015),” 2017. https://bhw.hrsa.gov/sites/default/files/bureau-health-workforce/data-research/diversity-us-health-occupations.pdf.
[xvii] Wyse, Rhea, Wei-Ting Hwang, Awad A. Ahmed, Erica Richards, and Curtiland Deville. “Diversity by Race, Ethnicity, and Sex within the US Psychiatry Physician Workforce.” Academic Psychiatry 44, no. 5 (October 1, 2020): 523–30. https://doi.org/10.1007/s40596-020-01276-z.
[xviii] Wilbur, Kirsten, Cyndy Snyder, Alison C. Essary, Swapna Reddy, Kristen K. Will, and Mary Saxon. “Developing Workforce Diversity in the Health Professions: A Social Justice Perspective.” Health Professions Education 6, no. 2 (June 1, 2020): 222–29. https://doi.org/10.1016/j.hpe.2020.01.002.
[xix] Cottonham, Danielle, and Amber Herrera. “What’s Causing the Shortage of Diverse Mental Health Providers?” Lyra Health, December 20, 2022. https://www.lyrahealth.com/blog/whats-causing-the-shortage-of-diverse-mental-health-providers/.
[xx] Sun, Ching-Fang, Christoph U. Correll, Robert L. Trestman, Yezhe Lin, Hui Xie, Maria Stack Hankey, Raymond Paglinawan Uymatiao, et al. “Low Availability, Long Wait Times, and High Geographic Disparity of Psychiatric Outpatient Care in the US.” General Hospital Psychiatry 84 (September 1, 2023): 12–17. https://doi.org/10.1016/j.genhosppsych.2023.05.012.
[xx] Bishop, Tara F., Matthew J. Press, Salomeh Keyhani, and Harold Alan Pincus. “Acceptance of Insurance by Psychiatrists and the Implications for Access to Mental Health Care.” JAMA Psychiatry 71, no. 2 (February 1, 2014): 181. https://doi.org/10.1001/jamapsychiatry.2013.2862.
[xxii] Satcher Health Leadership Institute, Eugene S. Farley, Jr. Health Policy Center, and Robert Graham Center. “The Economic Burden of Mental Health Inequities in the United States Report,” September 2022. https://satcherinstitute.org/wp-content/uploads/2022/09/The-Economic-Burden-of-Mental-Health-Inequities-in-the-US-Report-Final-single-pages.V3.pdf.
[1] At the time of publication, no comprehensive figure for the current economic cost of mental health could be found.
[xxiii] Insel, Thomas R. “Assessing the Economic Costs of Serious Mental Illness.” American Journal of Psychiatry 165, no. 6 (June 2008): 663–65. https://doi.org/10.1176/appi.ajp.2008.08030366.
[xxiv] The White House. “Reducing the Economic Burden of Unmet Mental Health Needs,” May 31, 2022. https://www.whitehouse.gov/cea/written-materials/2022/05/31/reducing-the-economic-burden-of-unmet-mental-health-needs/.
[xxv] Melek, Stephen, Douglas Norris, Jordan Paulus, Katherine Matthews, Alexandra Weaver, and Stoddard Davenport. “Potential Economic Impact of Integrated Medical-Behavioral Healthcare.” Milliman, January 2018. https://www.milliman.com/-/media/milliman/importedfiles/uploadedfiles/insight/2018/potential-economic-impact-integrated-healthcare.ashx.
[xxvi] The General Assembly of Pennsylvania. An Act Providing for Commonwealth support for a Mental Health and Intellectual Disability Staff Member Loan Forgiveness Program and an Alcohol and Drug Addiction Counselor Loan Forgiveness Program. HB2384.Referred to Committee on Human Services March 8, 2022, https://www.legis.state.pa.us/cfdocs/legis/pn/public/btCheck.cfm?txtType=HTM&sessYr=2021&sessInd=0&billBody=H&billTyp=B&billnbr=2384&pn=2803.
[xxvii] California Department of Health Care Access and Information. “Licensed Mental Health Services Provider Education Program (LMH).” Accessed October 16, 2023. https://hcai.ca.gov/loans-scholarships-grants/loan-repayment/lmhspep/.
[xxviii] Bärnighausen, Till, and David E. Bloom. “Financial Incentives for Return of Service in Underserved Areas: A Systematic Review.” BMC Health Services Research 9, no. 1 (May 29, 2009): 86. https://doi.org/10.1186/1472-6963-9-86.
[xxix] Elliott, Diana, and Miriam Farnbauer. “Bridging German and US Apprenticeship Models: The Role of Intermediaries.” Urban Institute, August 2021. https://www.urban.org/sites/default/files/publication/104677/bridging-german-and-us-apprenticeship-models.pdf.
[xxx] Ibid.
[xxxi] Health Care Apprenticeship Consortium. “Behavioral Health Apprenticeships,” n.d. https://healthcareapprenticeship.org/bh-apprenticeships/.
[xxxii] City College of San Francisco. “Community Health Worker Apprenticeship.” https://www.ccsf.edu/academics/career-education/community-health-worker-apprenticeship.
[xxxiii] Mauldin, Bronwyn. “Apprenticeships in the Healthcare Industry.” Skill Up Washington, 2011. http://skillupwa.nonprofitsoapbox.com/storage/documents/Apprenticeships_in_the_Healthcare_Industry.pdf.
